Lower Limb Rotation Deformities: Causes and Treatment
Lower limb rotational deformities are orthopedic conditions caused by abnormal twisting of the hip, thigh (femur), or shin (tibia) bones around their own axes. This alters an individual’s walking pattern, foot placement, and joint mechanics. Frequently detected in childhood as "in-toeing" or "out-toeing," these deformities, if left untreated, can contribute to joint degeneration and chronic pain in adulthood.
Accurate diagnosis is essential for successful treatment of patients with lower limb rotational deformities. Determining whether the issue stems from bone torsion or soft tissue problems requires thorough clinical and radiological assessment. This article reviews the causes of leg twisting, diagnostic methods, and current treatment options based on scientific evidence.
What Are Lower Limb Rotational Deformities?
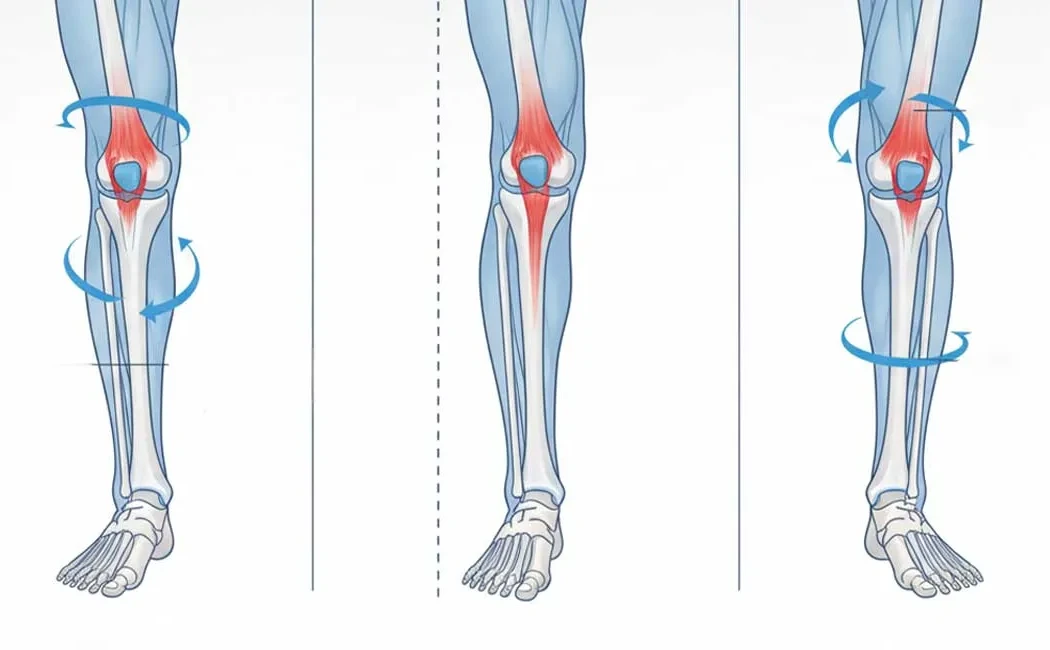
These deformities occur when leg bones deviate from their normal anatomical axes in the transverse (horizontal) plane. During normal development, children’s leg bones undergo specific rotational changes. However, when these changes exceed normal limits or present asymmetrically, they are considered pathological. The most common types are femoral anteversion (excessive inward twisting of the thigh bone) and tibial torsion (inward or outward twisting of the shin bone).
Such deformities are not only cosmetic concerns but also biomechanical problems.
Causes of Leg Twisting and In-Toeing Gait
Leg twisting may be congenital or develop during growth. Factors include intrauterine positioning (fetal constraint), genetic predisposition, and neuromuscular disorders. Conditions such as cerebral palsy, which affect muscle tone, can cause imbalanced muscle forces leading to rotational deformities.
In-toeing gait is a common parental concern and usually results from three main causes: metatarsus adductus in the foot, internal tibial torsion, or increased femoral anteversion. For more detailed information, please see our page on childhood lower limb deformities.
Metabolic disorders like vitamin D deficiency or rickets can also impair bone development and predispose to deformities. Early diagnosis and treatment of bone development disorders in children are vital to prevent permanent twisting.
Rotational Profile Analysis and Diagnostic Process
Comprehensive physical examination is fundamental for accurate diagnosis. The physician observes the patient’s walking and performs a series of measurements called "rotational profile analysis." This includes assessing hip rotation angles, thigh-to-foot alignment, and foot shape. The patient is typically examined lying prone to determine the degrees of femoral anteversion and tibial torsion.
In addition to physical exam, radiologic imaging is essential to quantify the deformity and visualize bone anatomy. Computed Tomography (CT) is especially useful for measuring transverse-plane bone rotation accurately. These measurements form the basis of surgical planning.
Treatment Options: Surgical and Non-Surgical Methods
Treatment strategy depends on the patient’s age, deformity severity, and how much symptoms interfere with daily life. Mild rotational deformities in children often improve spontaneously with growth. Regular monitoring and educating the family may be sufficient during this period.
Non-surgical options include targeted physiotherapy programs, modifying sitting postures (such as avoiding the "W-sitting" position), and infrequent use of orthoses. However, clinical evidence indicates that shoe modifications or braces have limited effect on correcting bone rotation.
Surgery is considered in adults or severe pediatric cases that do not resolve. Decisions for surgery take into account pain, frequent falls, walking difficulty, and cosmetic concerns. Corrective procedures aim to preserve joint health by preventing future arthritis, as outlined in our section on joint-preserving surgeries.
Surgical Techniques in Lower Limb Deformity Correction
The primary goal of surgery is to restore anatomical bone alignment and ensure proper joint function. The most common method is "derotation osteotomy," wherein the bone is surgically cut, rotated to the correct angle, and stabilized with plates, screws, intramedullary nails, or external fixators.
In complex cases or when limb length discrepancy coexists, lower limb deformity surgery can be combined with bone lengthening surgery. Ilizarov or computer-assisted external fixators (hexapod systems) allow simultaneous correction of rotation and length.
Postoperative Rehabilitation and Recovery
Recovery varies depending on the surgical technique and individual patient factors. Typically, patients begin mobilization on the day after surgery but are advised to avoid full weight-bearing until bone healing is sufficient. Crutches or walkers are used as support during this period.
Rehabilitation focuses on maintaining joint mobility and strengthening muscles. Professional physiotherapy during postoperative rehabilitation accelerates return to normal activities. Once bone union is confirmed radiographically (usually within 6–12 weeks), gradual return to sports and full activity is permitted.
Complications and Follow-Up
As with any surgery, risks include potential infection, nerve injury, or vascular damage, though these are uncommon. Delayed or nonunion of the bone is more frequent in smokers or patients with metabolic disorders.
Revision surgery may be required for malunion or delayed healing. For more information on managing these complications, please see our pages on malunion surgery and advanced treatments for nonunion fractures.
The information provided is for general informational purposes only and does not constitute medical advice. This content is not a substitute for individual diagnosis, treatment, or consultation. Diagnosis and treatment should only be determined following an in-person examination by a qualified healthcare professional. Since each patient's clinical condition is unique, surgical or non-surgical treatments may vary accordingly. The information is based on current scientific evidence and up-to-date medical practices.