Nonunion Issues in Femur Fractures and Surgical Approaches
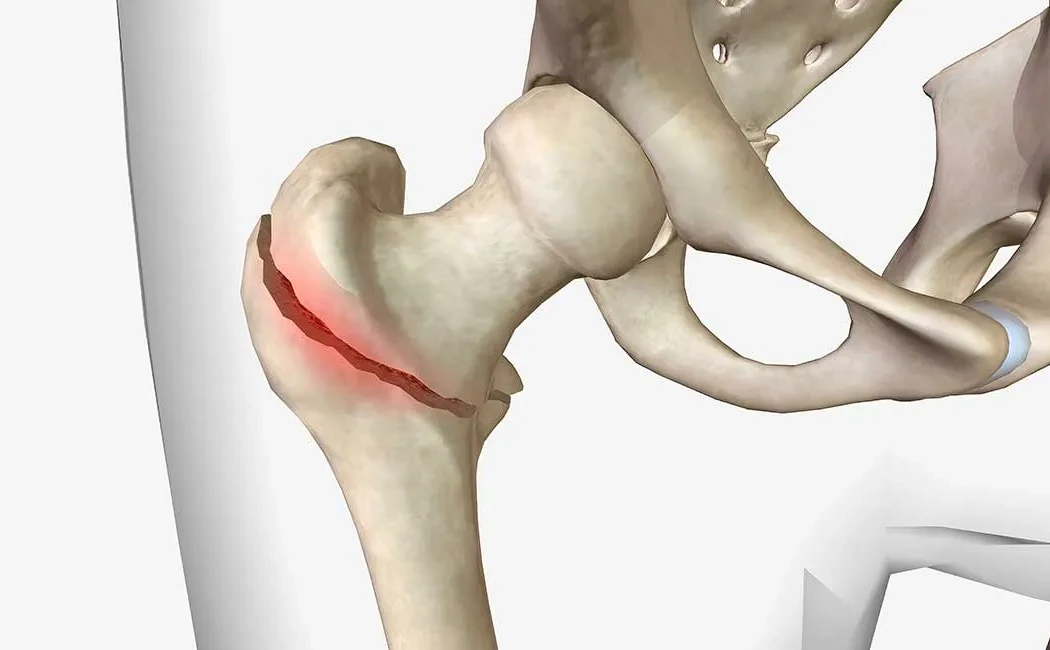
The femur is one of the longest and strongest bones in the body, and fractures due to trauma can lead to serious health complications. Femur fractures typically result from high-energy trauma and, if not properly treated, can result in nonunion—a condition where the bone ends fail to heal completely or take longer than expected to heal. Nonunion causes pain, limited movement, and functional loss in the patient.
Several factors contribute to nonunion, including surgical technique errors, inadequate stabilization, infection, impaired blood circulation, advanced age, smoking, systemic diseases, and weak mechanical forces at the fracture site. This risk is especially high in large bone fractures like the femur. Microscopic movements at the fracture line negatively affect osteogenesis and can lead to nonunion. Furthermore, in open fractures or cases with significant soft tissue damage, the risk of infection increases, which adversely impacts healing.
Diagnosis of nonunion involves clinical examination and imaging techniques. Patients often experience persistent localized pain at the fracture site and difficulties in walking and performing daily activities. X-rays reveal whether the fracture line remains open or if there are absent bone bridges. Advanced imaging techniques such as computed tomography (CT) or magnetic resonance imaging (MRI) may be employed for a detailed assessment of the bone and surrounding tissues.
When nonunion develops in a femur fracture, surgical treatment options vary depending on the patient's condition and the nonunion type. General strategies include replacing osteosynthesis materials, applying bone grafts, and performing debridement if infection is present. Different techniques address the mechanical and biological causes of nonunion.
If stability is lacking, revision of the existing plate or intramedullary nail is necessary to ensure good contact between bone ends and immobilization. The bone healing process is accelerated by supporting the nonunion site with autograft bone harvested from the iliac crest or other sites. Autografts stimulate osteoblast activity and promote new bone formation.
Infected nonunions require surgical cleaning (debridement) and appropriate antibiotic therapy. Temporary external fixators may be used to control infection in some cases. Once ideal conditions are achieved, permanent osteosynthesis devices are utilized for internal stabilization.
External fixator systems like the Ilizarov method are favored especially in complicated cases requiring deformity correction alongside the nonunion treatment. This technique uses rings and wires to control bone ends and applies mild distraction or compression forces to promote widespread bone healing.
Recently, supportive methods enhancing bone biology such as growth factors (BMP - bone morphogenetic proteins) and cellular therapies have been used as adjuncts in nonunion treatment. These approaches improve the bone's capacity to regenerate and increase surgical success rates.
Ultimately, nonunion in femur fractures requires a multidisciplinary approach. Careful evaluation of patient characteristics, fracture type, and causes of nonunion guide the surgical planning. When effective stabilization, infection control, and biological support are achieved, the chances of recovery significantly increase.