Current Approaches in Hip Replacement: Which Patients Are Recommended?
Hip replacement surgery is a critical orthopedic intervention aimed at improving quality of life and relieving pain in patients suffering from severe damage to the hip joint. Thanks to technological advances and novel surgical techniques, the success rates of hip replacement procedures have increased, and recovery times have accelerated. This article will explore current approaches in hip replacement and scientifically analyze which patient groups are suitable candidates for this treatment.
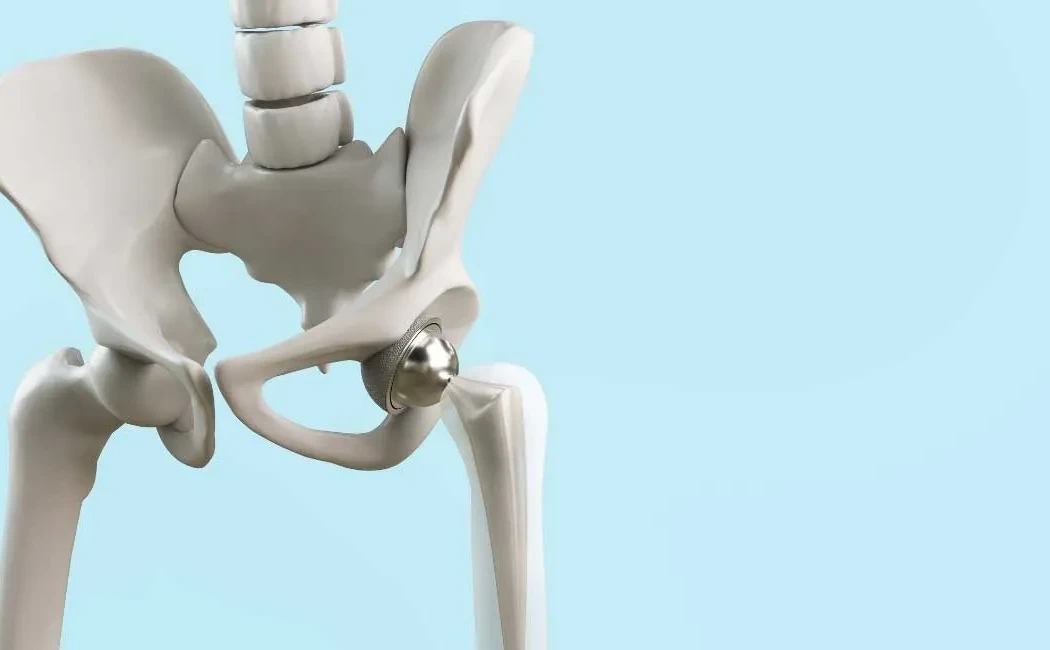
What is Hip Replacement and Why Is It Performed?
Hip replacement involves replacing the damaged hip joint with an artificial joint. It is commonly performed in cases of advanced osteoarthritis, rheumatoid arthritis, degenerative changes after trauma to the hip joint, aseptic necrosis, and certain tumorous conditions. The objective is to reduce pain, enhance functional mobility, and enable patients to resume daily activities.
Current Hip Replacement Techniques
Surgical approaches have diversified with advancing technology, offering patient-specific options. Modern methods include minimally invasive surgery, robot-assisted procedures, and advanced imaging techniques. These approaches aim to minimize tissue damage and accelerate recovery. Furthermore, durable and biocompatible materials such as ceramic, titanium, and polyethylene used in prostheses extend the implant’s lifespan.
Patient Selection and Indications
Selecting appropriate patients for hip replacement is vital for surgical success. Indications generally include:
- Severe hip pain and restricted movement
- Lack of response to conservative treatments (medication, physical therapy)
- Radiological evidence of progressive degeneration in the hip joint
- Noticeable decline in quality of life and difficulty performing daily activities
- Suitable overall health status and manageable surgical risks
Most candidates for hip replacement are elderly patients, but younger individuals are increasingly being evaluated for surgery; in their case, the durability of the prosthesis and potential revision surgeries are carefully considered.
Preoperative Evaluation and Planning
A thorough preoperative assessment is essential for successful hip replacement. This includes reviewing the patient’s medical history, comorbidities, hip deformities, and bone quality. In osteoporosis patients with low bone density, the choice of prosthesis and surgical technique is particularly critical. Today, three-dimensional imaging and computer-assisted planning enable more precise prosthesis placement.
Postoperative Rehabilitation
The success of hip replacement surgery depends not only on surgical technique but also on appropriate rehabilitation. Early goals include reducing movement restrictions, strengthening muscles, and increasing joint range of motion. Physical therapy programs are tailored to each patient, leading to significant improvements in quality of life for most individuals.
Risks and Complications
As with any surgical intervention, hip replacement carries certain risks. Possible complications include infection, prosthesis loosening, dislocation, nerve injury, and thrombosis. Although these complications are rare, they require careful management. Modern surgical techniques and infection prevention measures help minimize these risks.
The Future of Hip Replacement Treatment
Ongoing research in biotechnology and materials science aims to lengthen the lifespan of hip prostheses and improve their compatibility with the body. Personalized prosthesis designs and the widespread adoption of robotic surgery are additional factors expected to enhance treatment outcomes.
Hip replacement surgery is an effective method to restore a pain-free, functional life for patients when appropriate candidates are selected, precise surgical techniques are applied, and comprehensive rehabilitation is provided. Each patient’s clinical condition and expectations must be considered with a multidisciplinary approach to planning.